Pelvic Pain in Pregnancy

Being pregnant is one of the most joyful experiences in a woman’s life. To give birth to a new life is a wonderful miracle! Those littlest feet make the biggest footprints in our hearts.
Pregnancy brings on changes in the body, mind and life. The changes associated with pregnancy are physiological, i.e. normal. Hormonal fluctuations, increased blood volume, and weight gain all prepare the body for nurturing new life.
The pelvis comprised of the two hip bones, sacrum, coccyx, and pubic bone—undergoes significant change. The female pelvis is wider and more open to facilitate childbirth. One critical part of the pelvis is the pubic symphysis, a joint at the front of the pelvis that can become unstable during pregnancy. Pubic Symphysis helps to stabilize the pelvis and absorb shocks during movement and physical activities such as running. Ligaments hold the joint in place so that the pelvic bones can’t move unevenly or shift past the point of comfort
What is Pelvic Girdle Pain (PGP)?
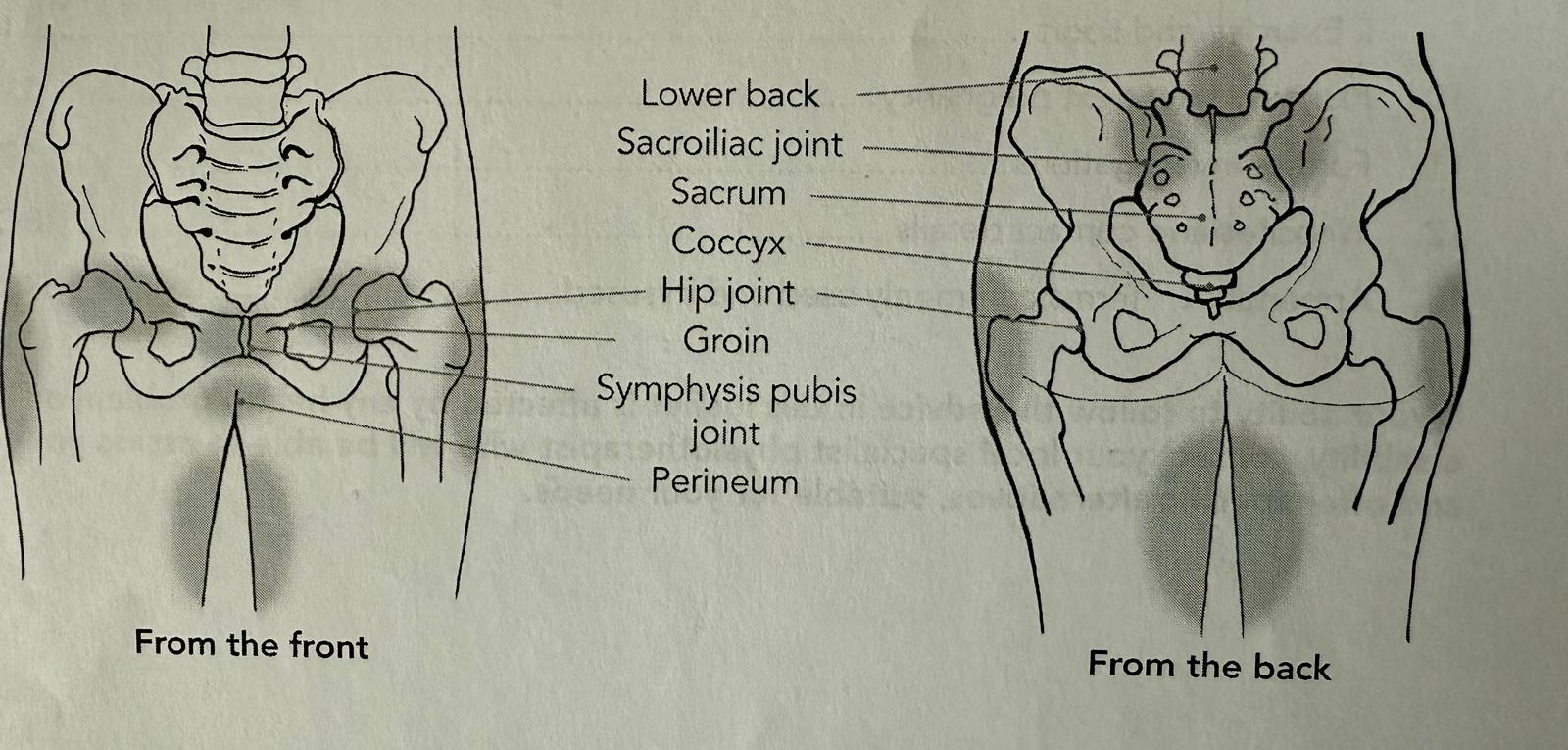
PGP is the term used to describe pain experienced in the front and the back of the pelvis, It is the pain in the joints that make your pelvic girdle, the symphysis pubic joint at the front and the left and right sacroiliac joints at the back. The pain is often experienced at the front below the tummy over the pubic bone or across one side of the lower back or both sides.
Causes of PGP
There is generally more than one factor involved in causing PGP:
- Uneven movement of the joints of the pelvic girdle.
- A change in the muscle activity that form the pelvic girdle, i.e. the muscles of the hip, pelvic floor, the lower abdomen. This can make the pelvic girdle less stable and trigger pain.
- A previous injury to the pelvis.
- Change in hormones during pregnancy.
- A history of previous low back pain and PGP
- More than one pregnancy
- Physically demanding/awkward work conditions/poor working postures
- High Body Mass Index (BMI) prior to pregnancy
During pregnancy, there are specific hormones produced in the body to relax the ligaments muscles and joints. Especially the hormone relaxin helps the ligaments to loosen, to accommodate the growing baby in the uterus. It also relaxes the abdominal muscles and helps the body stretch. For some women, this can lead to increased mobility at the joint, this coupled with the other factors can cause PGP. Due to the sharp pain experienced on movements around the symphysis pubis sometimes its referred as lightening crouch.
Concerns & Myth Busters
- About 1 in 5 pregnant women experience SPD.
- Having some pain does not imply that it will worsen with advancing pregnancy.
- It does not harm the baby but can significantly affect the quality of life for the mother to be.
- With the professional advice and treatment, especially during early pregnancy, PGP can be managed very well.
- If not treated appropriately during pregnancy, in a small percentage of women, the symptoms of PGP can linger after the childbirth.
Symptoms of PGP
- Pain at the pubic symphysis or in the lower back
- Radiating pain to groin, back, or thighs
- Difficulty walking, painful hip movements e.g. turning over in bed
- Pain with standing on one leg e.g. dressing, getting in and out of the bath, climbing stairs
- Difficulty in lying in some positions, e.g. side lying.
- Clicking or grinding in the pelvic region
- Pain and difficulty during sexual intercourse.
Severity can range from mild discomfort to disabling pain that affects work, sleep, and quality of life.
Diagnosis and Differentiation
A thorough assessment by a Pelvic Health Specialist Physiotherapist is a key to rule out:
- Other spine issues
- Urinary tract infection
- Muscular spasms
- Inflammation of the pubic symphysis
Our Pelvic Health expert clinicians at The Sherwood Clinic can help you diagnose and manage this pain effectively during pregnancy. The assessment will include a careful examination of your pelvic, back and hip joints as well as the muscles around them. We will assess your joint movements and the strength of the muscles as well as your walking pattern.
Comprehensive Treatment Options
Advice and Education
- Back care and lifting techniques
- Positions for labour and birth
- Lifting and handling of the baby and any toddlers
- Positions for sexual intercourse
Exercise and Specific Therapies
- Specific exercises to train your deep abdominal, hip and pelvic floor muscles
- Manual therapy for sacroiliac and pubic joints
- Soft Tissue Release Techniques for pain relief
- TENS (Transcutaneous Electrical Nerve Stimulation) for pain relief
- Clinical Pilates-based movements
- Breathing and relaxation techniques
- Stability platforms and balance trainers for core engagement and posture
Lifestyle Modifications
- Avoid activities that trigger pain
- Use pelvic support belts if appropriate
- Modify posture and sleeping positions
- Plan activities to avoid fatigue
Alternative and Supportive Therapies
- Acupuncture (shown to reduce pain intensity)
- Water based exercises
- Kinesiology taping
- Use of walking aids when needed
New Insights and Evidence-Based Updates
- Postpartum Persistence
Up to 25% of women report lingering pelvic girdle pain postpartum, which may last up to a year. Follow-up care and postnatal physiotherapy are crucial for long-term recovery.
- Mental Health Aspect
There is a growing link between PGP and perinatal anxiety or depression due to chronic pain and mobility issues. Addressing emotional well-being alongside physical rehabilitation is now considered essential.
- Digital Physiotherapy and Apps
Platforms like MummaWell and NHS-supported tools now provide guided exercises and consultations online, especially helpful for women with limited access to in-person physiotherapy.
- Kinesiology Taping
Evidence supports the use of kinesiology tape over the lower abdomen and pelvis to reduce instability and pain. This is a safe, non-invasive option that can be self-applied after physiotherapist guidance.
- Improved Sleep Positioning
Using U-shaped pillows or placing a pillow between the knees and ankles helps maintain pelvic alignment, supporting better sleep and reducing night pain.
- Preventive Strengthening
Women planning to conceive benefit from building core stability, gluteal strength, and pelvic floor control. Preconception physiotherapy is a growing trend to prevent SPD
- Vitamin D and Joint Stability
Low levels of Vitamin D may contribute to joint laxity. Ensuring adequate intake via sunlight, diet, or supplements (with medical advice) may reduce the risk of PGP.
A Case Study of a Client treated for PGP at The Sherwood Clinic
Ms X, 29 years old, 30 weeks pregnant with her first child referred herself for Women’s Health Physiotherapy for her pelvic pain. She reported experiencing pain in the front pelvis and lower backsince 19 weeks of pregnancy which now was getting worse, she felt the pain more around the left groin(7/10 on Numeric Rating Scale [NRS]). and pain while turning in bed, getting into the car, and transitional movements.She reported to be slightly overweight prior to pregnancy and had commenced gym x2/week and to build stamina by walking 10,000 steps x2/week for about three months of pregnancy. She was working full time – her work was primarily desk based, and her exercise and fitness routine had virtually ceased since her pregnancy.
On examination she had slightly limping gait with reduced weight bearing on the left side. She had very poor core activation, close questioning revealed mild urinary incontinence especially on coughing and sneezing indicating pelvic floor muscle weakness. There was weakness in her left hip muscles compared to her right.
Her management included education and training on core muscle activation technique to help her pain and to engage them especially during transitional movements. Soft tissue techniques were applied to provide effective pain relief. Further session included specific guidance on pelvic floor muscle activation and strength training. She was guided into positions to alleviate pressure on her affected side. Ms X was since once a week. By week four, her NRS scale for pain was 4/10. She felt more informed and empowered to manage her daily routine. An ongoing exercise programme was provided to Ms X to continue and to have monthly follow-up for exercise/symptom management as required.
Take Home Message
Pregnancy need not be burdened with pain and fear. It’s important to learn about the changing needs of your body and the specific muscle activation and training. Guidance from a Pelvic Health physiotherapist is crucial. A thorough assessment would support your journey to a healthy, empowered, and comfortable pregnancy,childbirth and postnatal return to fitness. Why not get in touch by emailing ( info@sherwoodtherapy.co.uk) or call on 0208 869 0000 to book your assessment with our Pelvic Health Physiotherapist.